Abstract
INTRODUCTION: Recipients of allogeneic hematopoietic cell transplantation (HCT) routinely undergo diagnostic radiographic tests in the course of their transplant care. While concerns have been raised over the risk of mutagenic events resulting from such exposure to low-dose ionizing radiation, effects in immunocompromised post-HCT hosts are unknown. We thus sought to quantify radiation exposure from medical imaging in a large cohort of allogeneic HCT patients and to evaluate its impact on transplant outcomes.
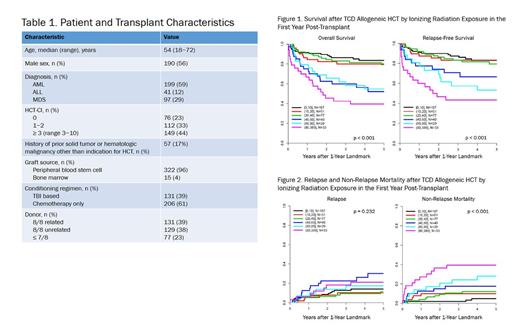
METHODS: This single-center retrospective study included recipients of first allogeneic HCT with T-cell depleted grafts for AML, ALL, or MDS from 2000 to 2013 who were alive at 1 year post-transplant. The analysis excluded patients who received a second allogeneic HCT before the 1-year landmark. All radiology exams performed in the first year post-HCT were tabulated. We then calculated total cumulative 1-year baseline radiation dosing for each patient using published estimates of doses corresponding to the individual imaging exams (National Council on Radiation Protection [NCRP] and Measurements, Publication No. 160, 2009; Kanal et al., Radiology 2017; Quinn et al., BMC Med Imaging 2016; Gao et al., BMC Med Imaging 2017). Overall survival (OS) and relapse-free survival (RFS) after the landmark were estimated by Kaplan-Meier methods. Relapse, non-relapse mortality (NRM), and development of late malignancies were estimated with the cumulative incidence method for competing risks. Association of categories of baseline radiation exposure with OS and RFS were evaluated using the logrank test, and associations with NRM, relapse, and late malignancy were evaluated using Gray's test.
RESULTS: A total of 476 patients underwent TCD HCT from 2000 to 2013, of whom 337 met eligibility criteria for the landmark analysis. Patient characteristics are shown in Table 1. The median number of radiographic tests in the first year was 9 (range 1-127), and median radiation exposure was 21.2 mSv (range 0.0-388.6; 1 mSv = 1 mGy). Given the wide range of radiation exposures, patients were divided into the following groups: 0-10 mSv of cumulative annual ionizing radiation (n = 107, 32%), 10-20 (n = 51, 15%), 20-40 (n = 77, 23%), 40-60 (n = 40, 12%), 60-80 (n = 29, 9%), and > 80 (n = 33, 10%). Across the entire cohort, OS was 78% (95% CI 73-82) at 2 years and 71% at 5 years (95% CI 66-76) after the 1-year landmark; RFS was 81% (95% CI 76-85) at 2 years and 74% (95% CI 69-79) at 5 years. Greater degrees of radiation exposure were associated with significantly poorer OS and RFS (Fig. 1). OS 2 years after the landmark, for instance, ranged from 45% (95% CI 31-66) in patients with > 80 mSv of radiation exposure to 90% (95% CI 84-96) in patients exposed to ≤ 10 mSv. Radiation exposure was also associated with significantly increased cumulative incidence of NRM (Fig. 2), which was, e.g., 40% (95% CI 22.4-57.0) at 2 years in patients exposed to > 80 mSv compared with 2% (95% CI 0.4-6.4) with ≤ 10 mSv. Cumulative incidence of relapse was 6.8% (95% CI 4.4-10.0) at 2 years and 10.4% (95% CI 7.2-14.3) at 5 years after the landmark. There was no significant association between radiation exposure and relapse (Fig. 2). As for late malignancies, cumulative incidence of secondary cancers or recurrence of prior cancers other than the indication for HCT was 2.4% (95% CI 1.1-4.5) at 2 years and 5.1% (95% CI 3.0-8.1) at 5 years after the landmark. Differences in radiation exposure were not significantly associated with development of such malignancies.
CONCLUSION: This is, to our knowledge, the first large-scale systematic quantification of ionizing radiation exposure after allogeneic HCT. Median radiation exposure from radiology exams alone in the first year post-transplant was more than 3 times the annual US average of 6.2 mSv from all causes as estimated by the NCRP, with a substantial number of patients exposed to upwards of 10 times this amount. Greater degrees of radiation exposure were associated with poorer survival and increased NRM, reflecting the more frequent use of diagnostic imaging among patients with post-transplant complications. However, radiation exposure did not correspond to significantly increased risk of relapse or late malignancy in this analysis.
O'Reilly: Atara: Patents & Royalties, Research Funding. van den Brink: PureTech Health: Consultancy; Jazz Pharmaceuticals: Consultancy; Seres: Research Funding; Therakos Institute: Other: Speaking engagement.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal